Get to Know How the Brain, Gut, and Dementia Are Related
Marco Aurélio Gomes Veado
3 min read
•
May 20, 2025
Many studies now suggest that an imbalanced gut microbiome, a condition known as dysbiosis, can trigger systemic inflammation, including inflammation in the brain. Chronic brain inflammation is considered a major contributor to cognitive decline and diseases like Alzheimer’s.
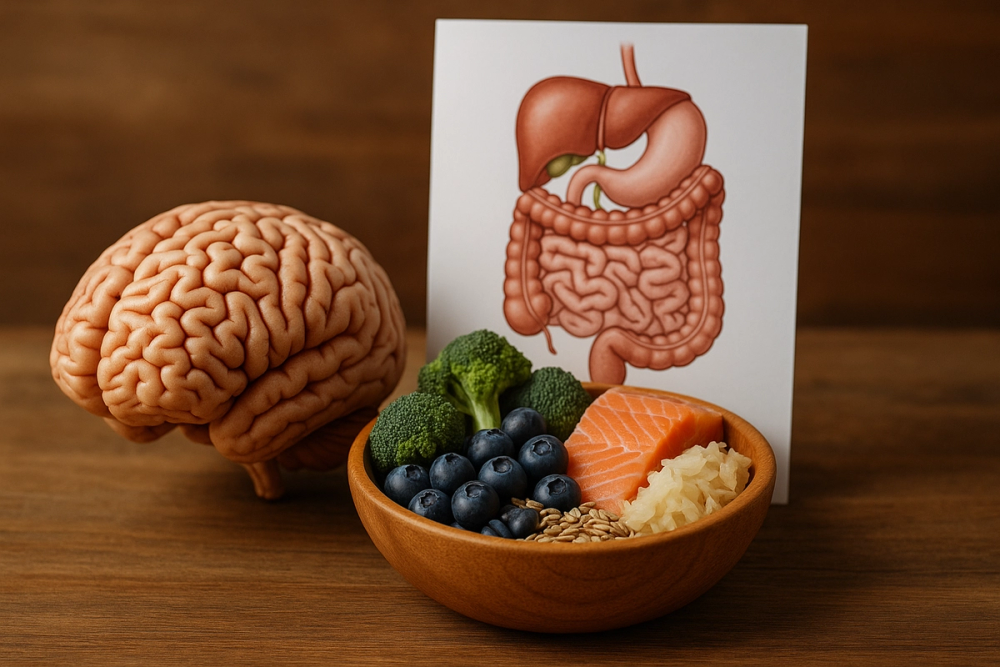
The gut-brain axis is a two-way communication network linking your digestive system to your brain. Understanding this powerful connection could offer new ways to prevent, manage, or even slow the progression of cognitive decline.
What Is the Gut-Brain Axis?
The gut-brain axis is the biochemical signaling that takes place between the central nervous system (CNS) and the enteric nervous system (ENS), often referred to as the body’s "second brain." This network uses the vagus nerve, immune system pathways, and even hormones to send information back and forth.
The gut is also home to trillions of microbes, collectively known as the gut microbiome. These tiny organisms are not just passengers; they play active roles in regulating inflammation, producing neurotransmitters like serotonin, and even influencing mood and cognition.
Gut Health and Inflammation: A Hidden Risk for Dementia
Many studies now suggest that an imbalanced gut microbiome, a condition known as dysbiosis, can trigger systemic inflammation, including inflammation in the brain.
Chronic brain inflammation is considered a major contributor to cognitive decline and diseases like Alzheimer’s.
Certain gut bacteria can produce toxins or pro-inflammatory molecules that leak into the bloodstream, cross the blood-brain barrier, and impact brain health. This might worsen memory, focus, and even accelerate neuronal death.
On the other hand, a healthy gut promotes anti-inflammatory responses and may help protect against neurodegeneration. Researchers have found differences in the gut microbiota composition between people with dementia and healthy individuals, suggesting a strong link between gut health and brain function.
Diet, Digestion, and Dementia Prevention
What you eat plays a critical role in shaping your gut microbiome and, by extension, your brain health. Diets rich in fiber, fermented foods, polyphenols, and omega-3 fatty acids (like the Mediterranean Diet) are associated with lower risks of dementia.
Key dietary tips to support both gut and brain health:
- Eat more prebiotics, like fiber-rich foods like bananas, garlic, and onions.
- Include probiotics such as ermented foods like yogurt, kefir, sauerkraut.
- Avoid ultra-processed foods high in sugar, additives, and unhealthy fats.
- Stay hydrated and aim for regular physical activity, which also supports gut diversity.
The Future: Gut-Based Therapies for Cognitive Decline?
New studies are testing probiotic supplements, fecal transplants, and gut-targeted medications as tools for managing dementia. While these therapies are still experimental, early results are promising.
Supporting the gut-brain connection may become a powerful part of future dementia care strategies, especially for people living with Mild Cognitive Impairment (MCI), a transitional stage that may lead to Alzheimer’s but can also be stabilized with the right interventions.
Conclusion
The brain and gut are in constant communication, and what happens in one deeply affects the other. As science uncovers more about this connection, individuals and caregivers can begin to take proactive steps to support brain health, starting with the gut.
At MCI and Beyond, we do believe in holistic, science-backed approaches to managing cognitive decline. Stay tuned to our biweekly newsletter for more insights, tips, and the latest research in dementia care.
Keywords: brain-gut dementia connection, gut microbiome and Alzheimer’s, inflammation and cognitive decline, gut-brain axis, mild cognitive impairment, dementia prevention diet
Sign up for our newsletter!
Get the latest information and inspirational stories for caregivers, delivered directly to your inbox.

